What if digital health could be built not just for data entry, but to empower community health workers and health officials to drive real-time action? This is the question guiding Khushi Baby, a digital health nonprofit based in India and a recipient of support through our corporate social responsibility program, Emergent GIVES.
In 2014, Khushi Baby began with a simple but powerful idea: a wearable health record for infants. In India, it’s common for mothers to return to their family homes for childbirth, often across village lines. Lacking a centralized system, community health workers struggled to track immunizations. Enter a culturally sensitive solution: instead of rubber wristbands or slips of paper, Khushi Baby embeds vaccination records into a traditional black thread bracelet (kala dhaaga) already worn by babies. This offline wearable record allowed community health workers (CHWs) to scan and update immunization data even when there was no internet access.
 Field visits soon revealed a broader truth to the team: CHWs were spending hours collecting data yet rarely saw that data used to support their work. They were caregivers without feedback, operating in silos with limited support. Today, it’s estimated that India’s CHWs lose around 50 million care hours every month to redundant reporting across fragmented systems. Many face delayed payments, limited supervision and a lack of tools to guide clinical decision-making.
Field visits soon revealed a broader truth to the team: CHWs were spending hours collecting data yet rarely saw that data used to support their work. They were caregivers without feedback, operating in silos with limited support. Today, it’s estimated that India’s CHWs lose around 50 million care hours every month to redundant reporting across fragmented systems. Many face delayed payments, limited supervision and a lack of tools to guide clinical decision-making.
In response, Khushi Baby began co-designing a system-wide solution with CHWs and state governments. The result was CHIP: the Community Health Integrated Platform.
Built over 250,000+ hours of fieldwork and co-design with CHWs and health officials, CHIP is grounded in a ‘3I’ strategy: Ink-free reporting, Incentive-linked performance and Integrated health programs and stakeholders. This strategy ensures that CHWs are equipped not just to collect data, but to act on it. Today, CHIP powers India’s largest state, Rajasthan.
CHIP equips CHWs with smartphone-based health applications and enables health officials to access dashboards for real-time insights. Together, they track over 800 indicators across 12 public health programs, spanning maternal and child health, tuberculosis, nutrition and emerging infectious diseases.
The investment in CHIP is all about translating data into action. When behavioral insights revealed that pregnant women were avoiding anemia care, Khushi Baby added one targeted survey question geared toward learning why. That single adjustment enabled follow-up care and improved outcomes, an example of how CHIP’s human-centered design leads to precision intervention.
CHIP was stress-tested during the COVID-19 pandemic, when the Government of Rajasthan enlisted Khushi Baby to lead the state’s digital health response. Within weeks, CHIP enabled:
- The first digital health census in the country
- AI-powered screening and triaging tools
- WhatsApp-based community outreach
- Deployment of over 50,000 health workers to screen 14 million residents during the first wave in 2020.
The crisis catalyzed CHIP’s evolution from a pilot to a platform. Today, CHIP is institutionalized in Rajasthan. It is now expanding to Karnataka and Maharashtra, with each state serving populations larger than most countries, with a goal to reach 100,000 CHWs and 100 million people by 2030.
CHIP is also paving the way for precision public health. Khushi Baby is developing:
- India’s first village-level Climate Health Vulnerability Index
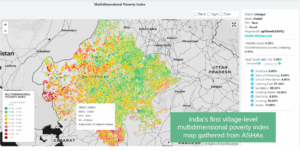
- A Multidimensional Poverty Index to guide targeted interventions
- Vector-borne disease dashboards for hotspot triaging
- Data diligence scores to track CHW performance and improve health worker support
Khushi Baby works as a technical partner to the government, not a vertical solution provider. This approach aids in translating CHIP data into actionable outcomes, whether it is predicting dengue outbreaks, tracking high-risk pregnancies, or mapping health service gaps.
In Rajasthan, CHIP is now the backbone of the State Digital Health Mission. Similar pathways are emerging in other states, enabling public-private financing and development partner alignment in a time when global health funding is under pressure.
Emergent’s support has strengthened the technical architecture and fueled research and innovation that makes precision health actionable in the real world.